The following tips can help your workforce reduce the risk of exposure to viruses. To learn more about our business response to COVID-19, visit https://www.afgroup.com/our-response-to-covid-19/.
These best practices have been developed from various sources and are intended to be used as resources only, and not to be relied upon as legal or official guidance. Individual companies are encouraged to refer to local and state requirements to determine the appropriate practices for their respective operations.
Additional Resources:
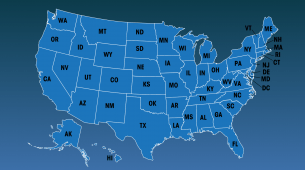
*New! Map: COVID Resources by State
(For best results view in Google Chrome.)
OSHA: www.osha.gov/coronavirus or 1-800-321-OSHA
OSHA ETS: https://www.osha.gov/coronavirus/ets
*NEW* OSHA Vaccine/Testing ETS: https://www.osha.gov/coronavirus/ets2
NIOSH: https://www.cdc.gov/niosh/emres/2019_ncov.html
CDC: www.cdc.gov/coronavirus/2019-nCoV/index.html
WHO: www.who.int/emergencies/diseases/novel-coronavirus-2019
Job Accommodation Network (JAN): https://askjan.org/
CPWR: https://www.cpwr.com/covid-19
AF Group Printable Resource: Returning to the Workplace COVID-19 – Precautions
Accident Fund: www.accidentfund.com/our-response-to-covid-19/
Accident Fund COVID-19 Claim Form
Infection Prevention Measures for all Industries
Determine what needs to be cleaned:
- Areas unoccupied for seven or more days require only normal routine cleaning.
- Outdoor areas generally require normal routine cleaning and do not require disinfection.
- Soft and porous materials that are not frequently touched should be cleaned/laundered following the directions on the label and using the warmest appropriate water setting.
- Visibly dirty surfaces should be cleaned prior to disinfection.
- Items frequently touched by multiple people (light switch, doorknob, toilet) should be cleaned and disinfected at least daily. More frequent cleaning and disinfection may be required based on level of use (carts or point of sale keypads) and should be completed before each use.
Cleaning and disinfection products:
- Follow EPA guidelines for which cleaning and disinfection products to use.
- Follow manufacturer guidelines for safe use and contact time for disinfection. Many products recommend keeping the surface wet for a specific amount of time.
- Safety data sheets and other manufacturer instructions can provide additional guidance on what PPE workers need to use the chemicals safely.
Personal protective equipment (PPE) and hand hygiene:
- The risk of exposure to cleaning staff is inherently low. Cleaning staff should wear disposable gloves, masks and gowns for all tasks in the cleaning process, including handling trash.
- Gloves and gowns should be compatible with the disinfectant products being used.
- Additional PPE might be required based on the cleaning/disinfectant products being used and whether there is a risk of splash. If gowns are not available, coveralls, aprons or work uniforms can be worn during cleaning/disinfecting. Reusable (washable) clothing should be laundered afterwards.
- After removing PPE, staff should wash their hands with soap and water for at least 20 seconds.
Additional considerations:
- Leave some doors open to reduce touching by multiple people.
- Open windows to improve ventilation.
- Remove objects in common areas (coffee creamer containers, mugs, etc.).
Helpful links
- CDC Reopening Guide – this web page provides a general framework for creating a cleaning and disinfection plan for your business (includes examples of frequently touched surfaces, instructions for cleaning soft surfaces like chairs and couches, etc.).
- CDC Disinfection Flow Chart – use this flow chart to determine what should be cleaned and how, based on location, occupancy and type of material.
- EPA-Registered Household Disinfectant List – this list contains products that meet the EPA’s criteria for use against the virus that causes COVID-19 – as well as the amount of time a surface should be visibly wet with each disinfectant.
- Monitor public health communications about COVID-19 recommendations for the workplace and ensure that workers have access to and understand that information.
- Encourage workers to stay home if they are feeling sick, have a fever, cough or shortness of breath or have been exposed to viruses.
- Survey applicants attending orientation about their wellbeing and any viral symptoms.
- Encourage respiratory etiquette, including covering coughs and sneezes.
- Promote frequent and thorough hand washing. Instruct employees to wash their hands with soap and water for at least 20 seconds or clean their hands often with an alcohol-based hand sanitizer that contains at least 60-95% alcohol.
- Educate workers about current precautions being taken at their facility or job site and actions they can take to protect themselves.
- Provide tissues, disinfectants and disposable towels that workers can use to clean high-touch work surfaces at the beginning and end of every shift, per CDC guidelines.
- Use Environmental Protection Agency-approved cleaning chemicals from List N.
- Discourage workers from sharing tools and equipment. Employees should especially not share headsets or other objects that are near their mouth or nose.
- Install hands-free door opener devices on restroom doors.
- Provide resources like helplines and Human Resources contacts for employees to manage their mental and emotional safety while working.
- Establish flexible work hours and allow office staff to work from home when feasible.
- Limit employee access to areas outside of the departments they work in.
- Encourage office employees to call coworkers on the phone, even if in the same department.
- Utilize alternative modes of communication for meetings and training when possible.
- Seek alternatives to physical punch cards and community pens for time clocks, roll call and other sign-in requirements.
- Practice sensible social distancing and maintain six feet between co-workers where possible.
- Provide or allow workers to wear personal protective equipment (PPE), like masks and gloves.
- Train workers on how to properly put on, use/wear, take off and maintain protective clothing and equipment.
On June 21, 2021, the U.S. Federal Register published OSHA’s COVID-19 Emergency Temporary Standard requiring that employers who provide direct care (health care, long term care, social services) develop and implement effective COVID-19 plans in the workplace. Find a highlight of these guidelines below.
- Develop and implement COVID-19 Plan
- Enforce patient screening and management
- Follow standard and transmission-based precautions
- Follow CDC guidelines for cleaning and disinfection
- Perform health screening and medical management before each workday/shift
- Follow the OSHA Employer Notification Tool guidelines to alert employees within 24 hours when a person who has been in the workplace is positive
- Follow requirements for removing employees from the workplace
- Provide medical removal protection benefits
- Provide reasonable time and paid leave for vaccinations and vaccine side effects
- Train employees on workplace COVID-19 policies and procedures using accessible formats and in a language they understand – ETS Employee Training Presentation
- Implement protections from retaliation
- Set up anonymous process for workers to voice concerns about COVID-19-related hazards
- Implement all requirements at no cost to employees
- Establish a COVID-19 recordkeeping log (if more than 10 employees) – Sample log
- Report work-related COVID-19 fatalities and in-patient hospitalizations to OSHA
For further information, review OSHA’s complete ETS guidelines.
OSHA released updated COVID-19 guidance for employers not covered by the June 2021 Emergency Temporary Standard. Find a highlight of these guidelines below.
- Follow CDC Interim Public Health Recommendations for Fully Vaccinated People
- Grant paid time off for employees to get vaccinated and recover from any vaccine side effects
- The following individuals should be instructed to stay home from work:
- Individuals infected with COVID-19
- Individuals with COVID-19 symptoms
- Unvaccinated individuals who have had close contact with a positive individual
- Implement physical distancing for unvaccinated and at-risk workers in communal areas
- Train employees using accessible formats and in a language they understand
- Training should include:
- Workplace COVID-19 policies and procedures
- Basic facts about COVID-19 spread and prevention
- Maintain ventilation systems per OSHA and CDC recommendations
- Perform routine cleaning and disinfection according to CDC recommendations
- Record and report COVID-19 infections and deaths
- Implement protections from retaliation
- Set up anonymous process for workers to voice concerns about COVID-19-related hazards
- Training should include:
Visit OSHA’s COVID-19 webpage for more information.
- Workstation Setup
- Computer Workstation Assessment
- Office Ergonomics eLearning Course
- Office Ergonomics Video
- Remote Worker Safety Tip Sheet
- Loss Control Services for Parcel Delivery Companies
- Guide to Establishing a Housekeeping Program
- Guide to Home Health Care Safety
- Guide to Janitorial Safety
- Removing Gloves Safely
- Pick-up and Delivery Safety
Industry-Specific Considerations
- Maintain six feet between co-workers and customers, where possible.
- Establish six-foot distances with floor tape for customer lines.
- If social distancing is a challenge at checkouts, consider opening only every other cash register, temporarily moving workstations to create more distance, and/or installing plexiglass partitions.
- Lock or limit access to public restrooms through a key request, if feasible, in order to monitor usage and clean appropriately.
- Install hands-free door opener devices on restroom doors and disinfect the restroom key.
- If you must move workers to different departments or job duties, ensure proper training of the new job tasks including all safety requirements.
- Implement a drive-through window or curbside pick-up.
- Encourage customers to use digital payment methods or pay with a card. Disinfect pens and cards accordingly.
- Provide workers and customers with tissues and trash receptacles.
- Maintain regular housekeeping practices, including routine cleaning and disinfecting of door handles, elevator buttons and railings, stair railings, remotes, phones, alarm clocks, lights (lamps and switches), key cards, condiment containers and other frequently touched surfaces.
- Require delivery drivers to remain in their vehicle during loading/unloading activities and utilize electronic shipping documents to minimize interactions.
- Encourage workers to change and wash their clothes when they get home from a job.
- Review CDC guidelines for schools and information from your state health department, county health department or district. Some school districts may be required to develop a written COVID-19 exposure plan.
- Educate staff and families about when to stay home and when they can return to school.
- Implement flexible sick leave policies and practices that enable staff to stay home when they are sick, have been exposed or are caring for someone who is sick.
- If feasible, conduct daily health checks (e.g., temperature screening and/or symptom checking).
- Teach and reinforce handwashing with soap and water for at least 20 seconds. If soap and water are not readily available, provide hand sanitizer that contains at least 60% alcohol.
- Encourage staff and students to cover coughs and sneezes with a tissue. Used tissues should be thrown in the trash and hands washed immediately.
- Teach and reinforce the use of cloth face coverings, especially when physical distancing is difficult.
- Support healthy hygiene behaviors by providing adequate supplies, including soap, hand sanitizer, paper towels, tissues, disinfectant wipes and no-touch/foot-pedal trash cans.
- Clean and disinfect frequently touched surfaces (e.g., playground equipment, door handles, sink handles, drinking fountains) within the school and on school buses at least daily or between use as often as possible. See CDC guidance for bus transit operators to clean and disinfect school buses or other transport vehicles.
- Use of shared objects (e.g., gym or physical education equipment, art supplies, toys, games, etc.) should be limited when possible or cleaned between use.
- Develop a schedule for increased, routine cleaning and disinfection.
- Ensure safe and correct use and storage of cleaning and disinfection products.
- Post signs in highly visible locations (e.g., school entrances, restrooms) that promote everyday protective measures and describe how to stop the spread of germs.
- Broadcast regular announcements on reducing the spread of COVID-19 on PA systems. Include messages about behaviors that prevent the spread of COVID-19 when communicating with staff and families.
- Ensure ventilation systems operate properly and increase the circulation of outdoor air as much as possible. For example, open windows and doors if doing so does not pose a safety or health risk.
- Install physical barriers, such as sneeze guards and partitions, particularly in areas where it is difficult for individuals to remain at least 6 feet apart (e.g., reception desks, between bathroom sinks).
- Provide physical guides, such as tape on floors or sidewalks and signs on walls, to create “one-way routes” in hallways and help maintain physical distance in lines.
- Have students and staff bring their own meals when feasible or serve individually plated meals in classrooms instead of in a communal dining hall or cafeteria.
- Avoid sharing food and utensils. Use disposable food service items (e.g., utensils, dishes, etc.) if feasible. Handle non-disposable food service items with gloves and wash them with dish soap and hot water or in a dishwasher.
- Use flexible worksites (e.g., telework) and flexible work hours (e.g., staggered shifts) to help establish policies and practices for social distancing.
- Pursue virtual group events, gatherings or meetings, if possible, and promote social distancing of at least 6 feet between people if events are held. Limit group size to the extent possible.
- Limit any nonessential visitors, volunteers and activities involving external groups or organizations – especially with individuals who are not from the local geographic area (e.g., community, town, city, county).
- Designate a staff person to be responsible for responding to COVID-19 concerns. All school staff and families should know who this person is and how to contact them.
- Cross-train staff and create a roster of trained back-up staff.
- Train staff on all safety protocols. Conduct training virtually or ensure that social distancing is maintained during training.
*Please note, these are informational items taken from various sources on the topic. Prior to implementing, you should discuss with an expert based on individual circumstances.
- Ensure enough handwashing/sanitizing stations are available at the worksite.
- Educate workers about the current precautions being taken at job sites and actions they can take to protect themselves.
- Modify work schedules to stage/stagger work crews and reduce the total number of employees on a job site at any given time.
- Prior to residential/individual business service, ask customer screening questions about recent illness, symptoms and travel.
- Consider submitting inspections, certifications, invoices, and other required documentation electronically.
- Provide and encourage customer use of digital payment options.
- Seek alternatives to physical punch cards/community pens for time clocks, roll call and other sign-in requirements.
- Encourage workers to drive to worksites/parking areas alone instead of carpooling.
- Minimize interactions when picking up or delivering equipment/materials.
- Organize the placement of materials at the worksite to minimize movement and interactions.
- Require delivery drivers to remain in their vehicle and utilize electronic shipping documents.
- Discourage workers from sharing hand tools, power tools, measuring devices and other tools and equipment.
- Disinfect all surfaces that are touched regularly, including vehicle/equipment interiors (steering wheel, gear shift, instrument panels, etc.) at the beginning and end of shifts.
- Do not use a common water cooler.
- Encourage workers to physically distance when they take breaks together, bring food and water bottles from home and to not share food/utensils.
- Wear proper personal protective equipment (PPE), including masks, safety glasses and gloves.
- Encourage workers to change and wash their clothes when they get home from a job.
- If contracted to perform work in healthcare facilities, train your workers in Infection Control Risk Assessment (ICRA).
- Consider implementing a work-hardening program with decreased hours to start with – as employees may be out of ‘working condition.’ Substitute safety training for remaining hours of the shift.
- Ensure enough handwashing/sanitizing stations are available at the worksite.
- Educate workers about the current precautions being taken on job sites and actions they can take to protect themselves.
- Modify work schedules to stage/stagger work crews and reduce the total number of employees on a job site at any given time.
- Prior to residential/individual business service, ask customer screening questions about recent illness, symptoms and travel.
- Consider submitting inspections, certifications, invoices, and other required documentation electronically.
- Provide and encourage customer use of digital payment options.
- Seek alternatives to physical punch cards/community pens for time clocks, roll call and other sign-in requirements.
- Encourage workers to drive to worksites/parking areas alone instead of carpooling.
- Minimize interactions when picking up or delivering equipment/materials.
- Organize the placement of materials to minimize movement on the worksite.
- Require delivery drivers to remain in their vehicle and utilize electronic shipping documents.
- Discourage workers from sharing hand tools, power tools, measuring devices and other electrical system maintenance tools and equipment.
- Disinfect all surfaces that are touched regularly, including vehicle/equipment interiors (steering wheel, gear shift, instrument panels, etc.) at the beginning and end of shifts.
- Do not use a common water cooler.
- Encourage workers to physically distance when they take breaks together, bring food and water bottles from home, and to not share food or utensils.
- Wear proper personal protective equipment (PPE), including masks, safety glasses and gloves.
- Encourage workers to change and wash their clothes when they get home from a job.
- If contracted to perform work in healthcare facilities, train your workers in Infection Control Risk Assessment (ICRA).
- Consider implementing a work-hardening program with decreased hours to start with – as employees may be out of ‘working condition.’ Substitute safety training for remaining hours of the shift.
- Encourage workers to report any safety and health concerns.
- Ensure enough handwashing/sanitizing stations are available at the worksite.
- Educate workers about the current precautions being taken on job sites and actions they can take to protect themselves.
- Modify work schedules to stage/stagger work crews and reduce the total number of employees on a job site at any given time.
- Prior to residential/individual business service, ask customer screening questions about recent illness, symptoms and travel.
- Consider submitting inspections, certifications, invoices and other required documentation electronically.
- Provide and encourage customer use of digital payment options.
- Seek alternatives to physical punch cards/community pens for time clocks, roll call and other sign-in requirements.
- Encourage workers to drive to worksites/parking areas alone instead of carpooling.
- Minimize interactions when picking up or delivering duct work, mechanical units and other equipment/materials.
- Organize the placement of materials to minimize movement on the worksite.
- Require delivery drivers to remain in their vehicle and utilize electronic shipping documents.
- Discourage workers from sharing hand tools, power tools, measuring devices, and other HVAC tools and equipment.
- Disinfect all surfaces that are touched regularly, including vehicle/equipment interiors (steering wheel, gear shift, instrument panels, etc.) at the beginning and end of shifts.
- Do not use a common water cooler.
- Encourage workers to physically distance when they take breaks together, bring food and water bottles from home and to not share food or utensils.
- Wear proper personal protective equipment (PPE), including masks, safety glasses and gloves.
- Encourage workers to change and wash their clothes when they get home from a job.
- If contracted to perform work in healthcare facilities, train your workers in Infection Control Risk Assessment (ICRA).
- Consider implementing a work-hardening program with decreased hours to start with – as employees may be out of ‘working condition.’ Substitute safety training for remaining hours of the shift.
- Encourage workers to report any safety and health concerns.
- Ensure enough handwashing/sanitizing stations are available at the worksite.
- Educate workers about the current precautions being taken at job sites and actions they can take to protect themselves.
- Modify work schedules to stage/stagger work crews and reduce the total number of employees on a job site at any given time.
- Prior to residential/individual business service, ask customer screening questions about recent illness, symptoms and travel.
- Consider submitting inspections, certifications, invoices, and other required documentation electronically.
- Provide and encourage customer use of digital payment options.
- Seek alternatives to physical punch cards/community pens for time clocks, roll call and other sign-in requirements.
- Encourage workers to drive to worksites/parking areas alone instead of carpooling.
- Minimize interactions when picking up or delivering piping and other equipment/materials.
- Organize the placement of materials to minimize movement on the worksite.
- Require delivery drivers to remain in their vehicle and utilize electronic shipping documents.
- Discourage workers from sharing hand tools, power tools, measuring devices and other plumbing tools and equipment.
- Disinfect all surfaces that are touched regularly, including vehicle/equipment interiors (steering wheel, gear shift, instrument panels, etc.) at the beginning and end of shifts.
- Do not use a common water cooler.
- Encourage workers to physically distance when they take breaks together, bring food and water bottles from home and to not share food or utensils.
- Wear proper personal protective equipment (PPE), including masks, safety glasses, gloves and face shields.
- Encourage workers to change and wash their clothes when they get home from a job.
- If contracted to perform work in healthcare facilities, train your workers in Infection Control Risk Assessment (ICRA).
- Consider implementing a work-hardening program with decreased hours to start with – as employees may be out of ‘working condition.’ Substitute safety training for remaining hours of the shift.
- Encourage workers to report any safety and health concerns.
- Seek alternatives to physical punch cards/community pens for time clocks, roll call and other sign-in requirements.
- Where social distancing is a challenge, consider limiting the duration of the activities, temporarily moving or repositioning workstations to create more distance, and/or installing plexiglass shields or other barriers between workstations.
- Establish protocols for disinfecting shared workspaces.
- Minimize interactions when picking up or delivering equipment or materials.
- Organize the placement of materials in work areas to minimize movement.
- Require delivery drivers to remain in their vehicle and utilize electronic shipping documents.
- Wear proper personal protective equipment (PPE), including masks, safety glasses and gloves. Plumbers should also consider wearing a full-face shield.
- Encourage workers to change and wash their clothes when they get home from a job.
- Consider implementing a work-hardening program with decreased hours to start with – as employees may be out of ‘working condition.’ Substitute safety training for remaining hours of the shift.
- Encourage workers to report any safety and health concerns.
- Conduct daily health screenings for caregivers at the beginning of their shift.
- Take patient’s temperature and ask screening questions to inquire about any recent illness, symptoms and travel.
- Conduct worksite assessments to identify exposure prevention strategies.
- Review current resident services and restrict non-essential healthcare personnel, such as elective consultations and volunteers, from providing in-home services.
- Consider implementing telehealth to offer remote access to care activities.
- Educate patients, their families and caregivers about COVID-19, how it spreads, risk of exposure and actions they can take to protect themselves.
- Provide supplies necessary to adhere to recommended infection prevention and control practices.
- Make necessary personal protective equipment (PPE) available to caregivers, including gloves, face masks and gowns that can be discarded or put into a storage container in the worker’s vehicle after each visit. Prioritize respirators for aerosol generating procedures.
- Train workers on how to properly put on, use/wear, take-off, and maintain protective clothing and equipment.
- Encourage staff to discard PPE, prior to leaving the patient’s residence or before entering their vehicle and to change and wash their clothes when they get home.
- Encourage caregivers to always wear a face mask or cloth face covering while they are in a patient’s residence. Guidance on extended use and reuse of face masks is available from the CDC. Cloth face coverings should NOT be worn instead of a respirator or face mask if more than source control is required.
- Remind patients to practice social distancing and perform frequent hand hygiene.
- Have patients wear a cloth face covering or face mask, when feasible.
- Provide alcohol-based hand sanitizer for caregivers to use before entering a residence and after leaving/entering their vehicle.
- Encourage the owners of residences to regularly clean and disinfect door handles, bed railings, wheelchairs, hand railings, remotes, phones, alarm clocks, lights (lamps and switches) and containers, and other frequently touched surfaces in common areas.
- Encourage workers to report any safety and health concerns.
- Encourage caregivers to stay home if they are feeling sick or have a fever, cough or shortness of breath.
- Evaluate and manage residents/patients and caregivers with a fever and symptoms consistent with COVID-19. Screen all caregivers at the beginning of their shift.
- Encourage respiratory etiquette, including covering coughs and sneezes.
- Make tissues and trash cans available in common areas and resident rooms for respiratory hygiene and cough etiquette and source control.
- Educate residents/patients, healthcare workers and visitors about the current precautions being taken in the facility and actions they can take to protect themselves.
- Dedicate space in the facility to monitor and care for residents/patients with COVID-19.
- Review current resident services and restrict non-essential healthcare personnel, such as elective consultations and volunteers, from providing in-home services.
- Consider implementing telehealth to offer remote access to care activities.
- Educate patients, their families and caregivers about COVID-19, how it spreads, risk of exposure and actions they can take to protect themselves.
- Provide supplies necessary to adhere to recommended infection prevention and control practices.
- Lock or limit access to public restrooms through a key request, if feasible, in order to monitor usage and clean appropriately.
- Install hands-free door opener devices on restroom doors and disinfect the restroom key.
- Make necessary personal protective equipment (PPE) available in areas where resident care is provided.
- Position a trash can near the exit inside the resident room to make it easy for staff to discard PPE, prior to exiting the room, or before providing care for another resident in the same room.
- Train workers on how to properly put on, use/wear, take-off, and maintain protective clothing and equipment.
- Encourage workers to always wear a face mask or cloth face covering while they are in the healthcare facility.
- If there are shortages of face masks, prioritize them for health care workers and then for residents/patients with symptoms (as supply allows). Prioritize respirators for aerosol generating procedures. Guidance on extended use and reuse of face masks is available from the CDC. Cloth face coverings should NOT be worn instead of a respirator or face mask if more than source control is required.
- Remind residents/patients to practice social distancing and wash hands frequently.
- Have residents/patients wear a cloth face covering or face mask whenever they leave their room, if feasible, including for procedures outside of the facility.
- Put alcohol-based hand sanitizer in every resident/patient room (ideally both inside and outside of the room) and other resident care and common areas.
- Develop a schedule for regular cleaning and disinfection of door handles, call buttons, bed railings, wheelchairs, elevator buttons and rails, hand railings, remotes, phones, alarm clocks, lights (lamps and switches), key cards, containers, shared equipment and other frequently touched surfaces in resident rooms and common areas.
- Encourage workers to report any safety and health concerns.
- Limit access to the maintenance facility and other departments only to employees who work in those areas.
- Minimize interpersonal interaction by working with customers to allow drivers to remain in their vehicle during loading/unloading activities and by utilizing electronic shipping documents.
- Provide and encourage the use of masks and gloves by drivers when at customer facilities.
- Survey drivers attending orientation about their wellbeing and any viral symptoms.
- Provide tissues, disinfectants and disposable towels that workers can use to clean office work surfaces and vehicle interiors (steering wheel, gear shift, instrument panels, etc.) at the beginning and end of every shift.
Share this resource:
URL coppied to clipboard.
Or send it directly to someone via our email form: